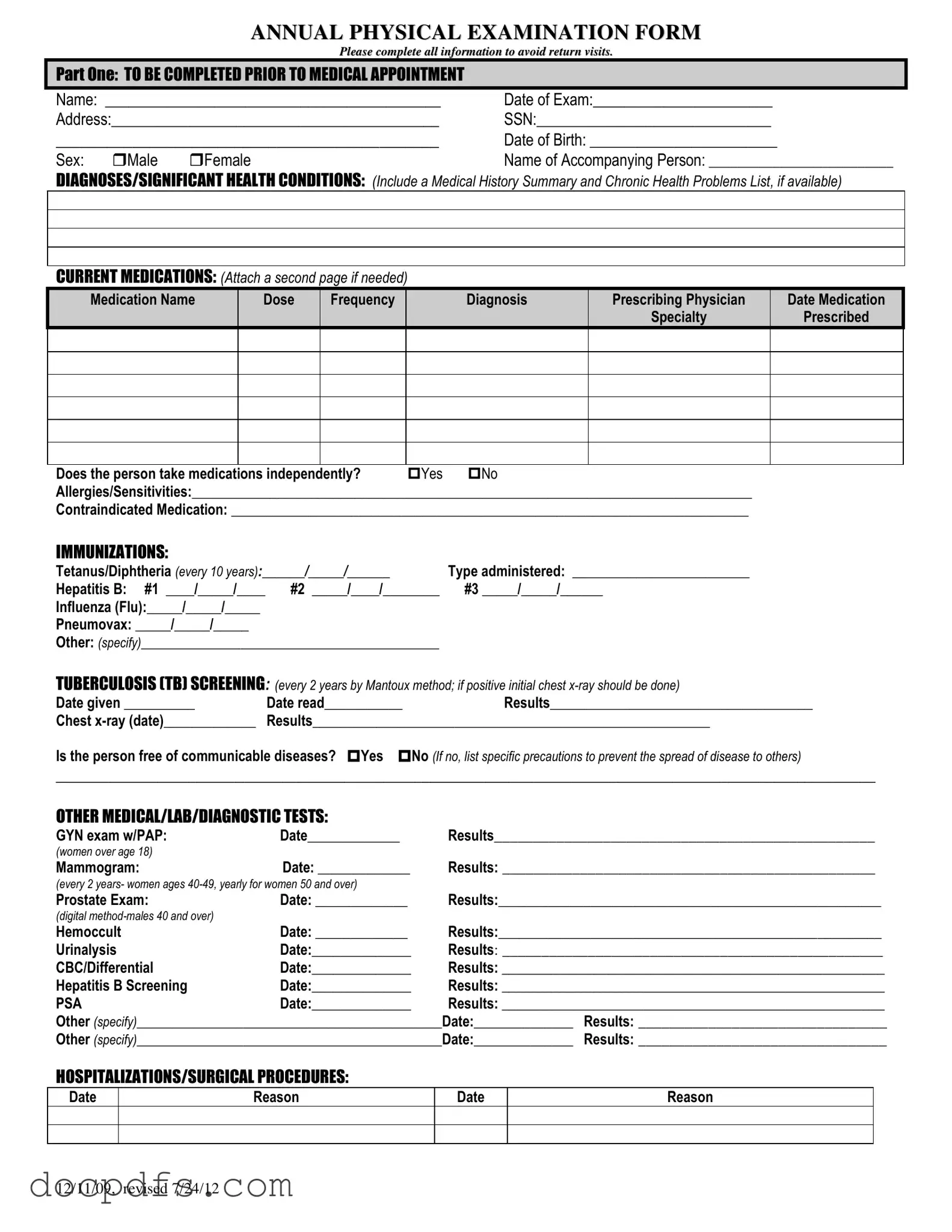
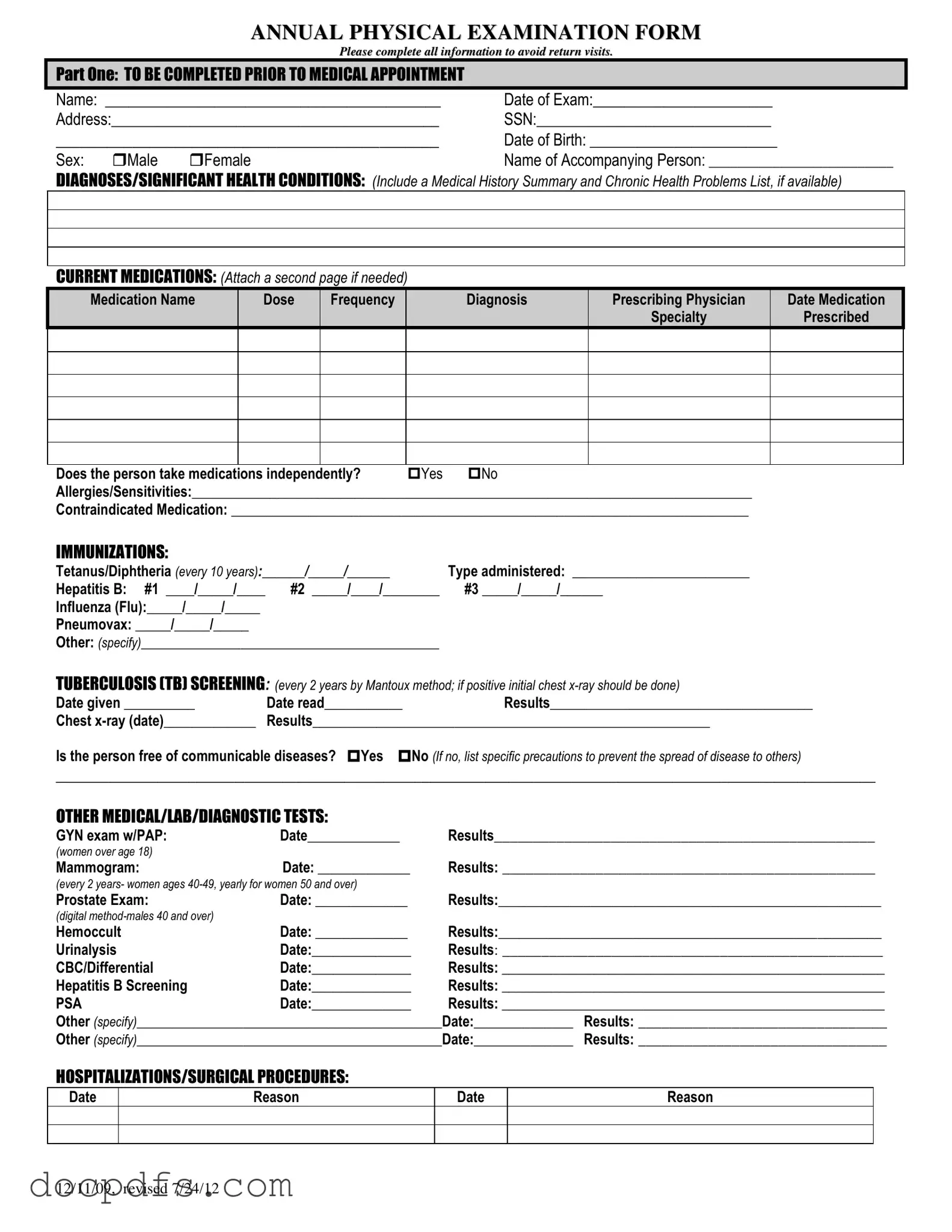
The Annual Physical Examination form is designed to gather essential health information about an individual prior to their medical appointment. This information helps healthcare providers assess the patient’s overall health, identify any existing conditions, and plan appropriate care. Completing this form thoroughly can minimize the need for follow-up visits, ensuring a more efficient healthcare experience.
Part One of the form requires personal details such as the patient's name, date of birth, address, and Social Security Number. Additionally, it asks for information about current medications, allergies, immunizations, and any significant health conditions. Providing a complete medical history summary and a list of chronic health problems is also encouraged to give the healthcare provider a clearer picture of the patient's health status.
How should I list my current medications?
When listing current medications, include the medication name, dosage, frequency of intake, the diagnosis for which it was prescribed, the prescribing physician's name, and the date it was prescribed. If you are taking multiple medications, feel free to attach an additional page if necessary. It is also important to indicate whether the individual takes medications independently.
The form requires documentation of several immunizations, including:
-
Tetanus/Diphtheria (every 10 years)
-
Hepatitis B (three doses)
-
Influenza (annual)
-
Pneumovax (as recommended)
Any additional immunizations should also be specified. Keeping this information up to date is crucial for preventive health measures.
What should I do if I have allergies or sensitivities?
If you have allergies or sensitivities, you should clearly list them in the designated section of the form. This information is vital for healthcare providers to avoid prescribing medications or treatments that could trigger an allergic reaction. Additionally, if there are any contraindicated medications, those should also be noted to ensure patient safety.
What happens if I have a history of communicable diseases?
If you have a history of communicable diseases, you must indicate this on the form. You will also need to specify any precautions that should be taken to prevent the spread of disease to others. This information allows healthcare providers to take necessary steps to protect both the patient and others in the healthcare setting.
Part Two focuses on the general physical examination. It includes vital signs such as blood pressure, pulse, and temperature, as well as a comprehensive evaluation of various body systems. The healthcare provider will assess whether findings are normal and may provide comments or recommendations for further evaluation if necessary. This section helps in identifying any immediate health concerns that may require attention.