What is a Do Not Resuscitate (DNR) Order?
A Do Not Resuscitate Order is a legal document that allows a person to refuse resuscitation efforts in the event of cardiac arrest or respiratory failure. This means that if a person stops breathing or their heart stops beating, medical personnel will not perform CPR or other life-saving measures.
Who can request a DNR Order?
A DNR Order can be requested by a patient who is capable of making their own medical decisions. If the patient is unable to communicate their wishes, a legally authorized representative, such as a family member or healthcare proxy, may request the order on their behalf.
How do I obtain a DNR Order?
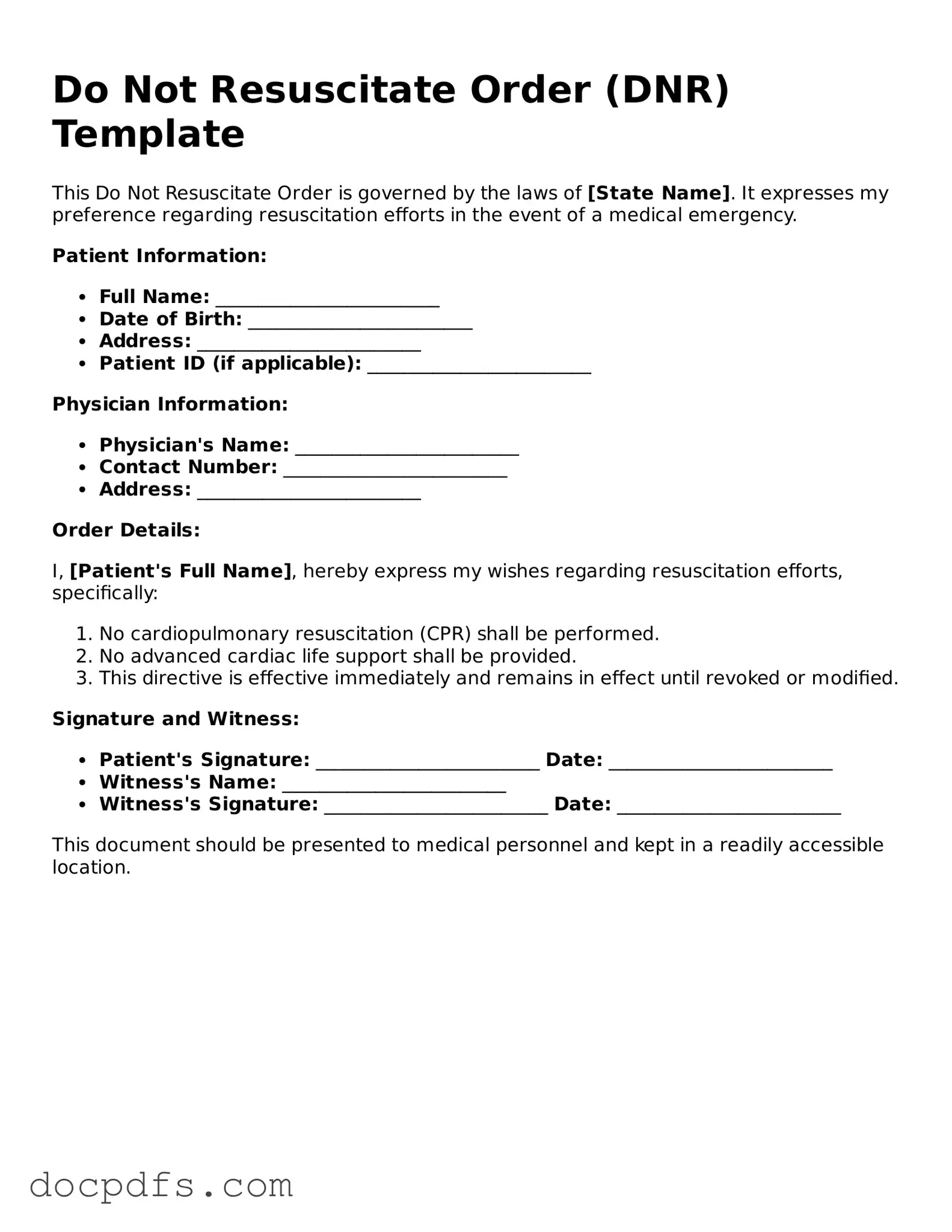
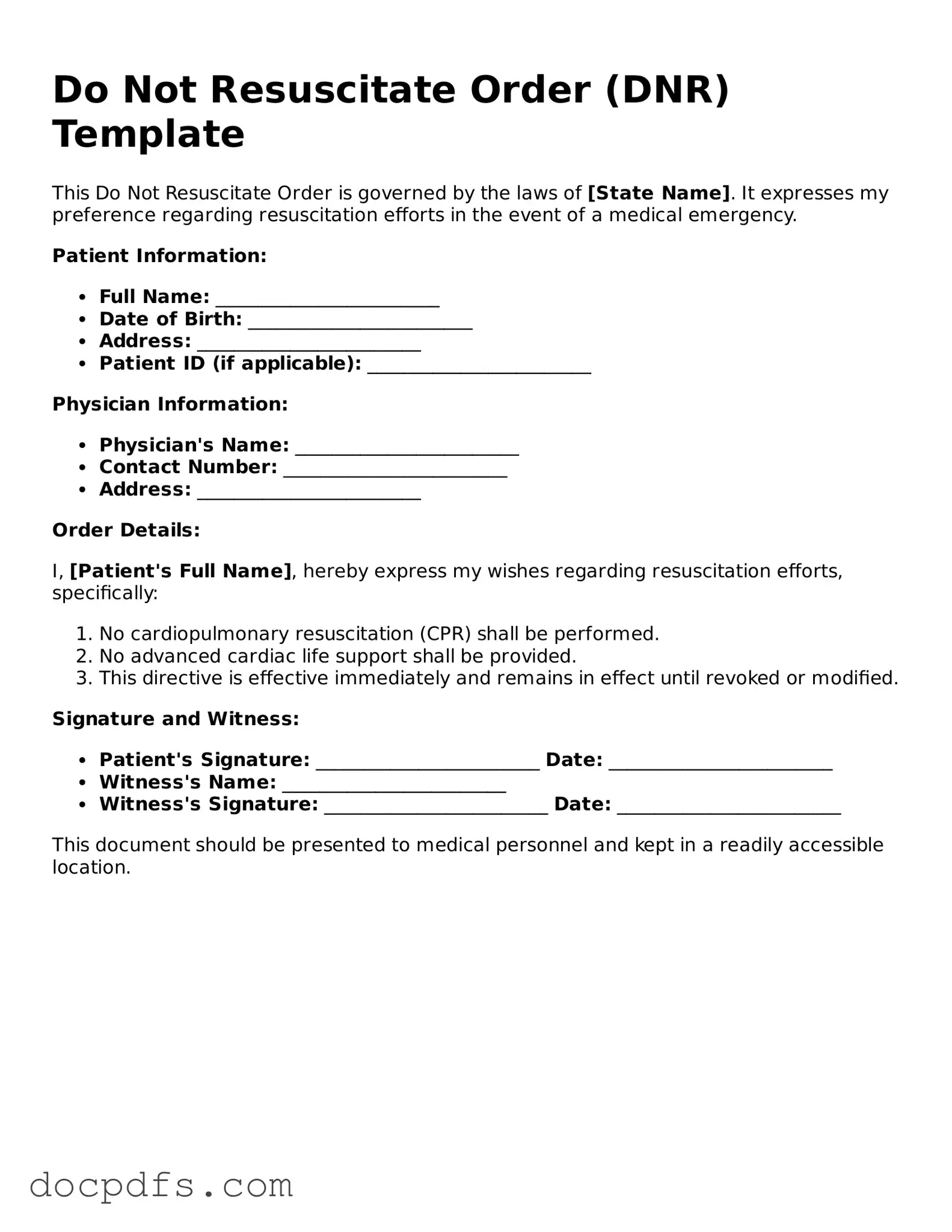
To obtain a DNR Order, follow these steps:
-
Consult with your healthcare provider about your wishes regarding resuscitation.
-
Complete the DNR Order form, which may be provided by your healthcare facility or can often be found online.
-
Ensure the form is signed by you and your healthcare provider.
-
Distribute copies of the signed order to your healthcare team, family members, and keep a copy for yourself.
Is a DNR Order the same as an Advance Directive?
No, a DNR Order is not the same as an Advance Directive. While both documents express a person's wishes regarding medical treatment, an Advance Directive is broader. It may include decisions about various medical treatments, not just resuscitation. A DNR Order specifically addresses the issue of resuscitation efforts.
Can a DNR Order be revoked?
Yes, a DNR Order can be revoked at any time. If you decide to change your mind, simply notify your healthcare provider and destroy any copies of the DNR Order. It is essential to communicate your decision to your family and healthcare team to ensure they are aware of your current wishes.
Will a DNR Order affect other medical treatments?
A DNR Order only applies to resuscitation efforts. It does not affect other medical treatments or interventions. You will still receive appropriate medical care, including pain management and comfort measures, even if you have a DNR Order in place.
How is a DNR Order recognized across different healthcare settings?
Most healthcare facilities are required to recognize a valid DNR Order. However, it is crucial to ensure that the order is properly documented and communicated. Carrying a copy of the order with you can help ensure that your wishes are honored in various settings, such as hospitals, nursing homes, or during emergency situations.
Can family members override a DNR Order?
Generally, family members cannot override a valid DNR Order if it was signed by the patient or their legally authorized representative. However, family discussions about end-of-life wishes are important. Open communication can help avoid confusion and ensure that everyone understands the patient's preferences.
What should I do if I have questions about my DNR Order?
If you have questions or concerns about your DNR Order, it is best to speak with your healthcare provider. They can provide clarity on the order, explain its implications, and help you make informed decisions about your healthcare preferences.