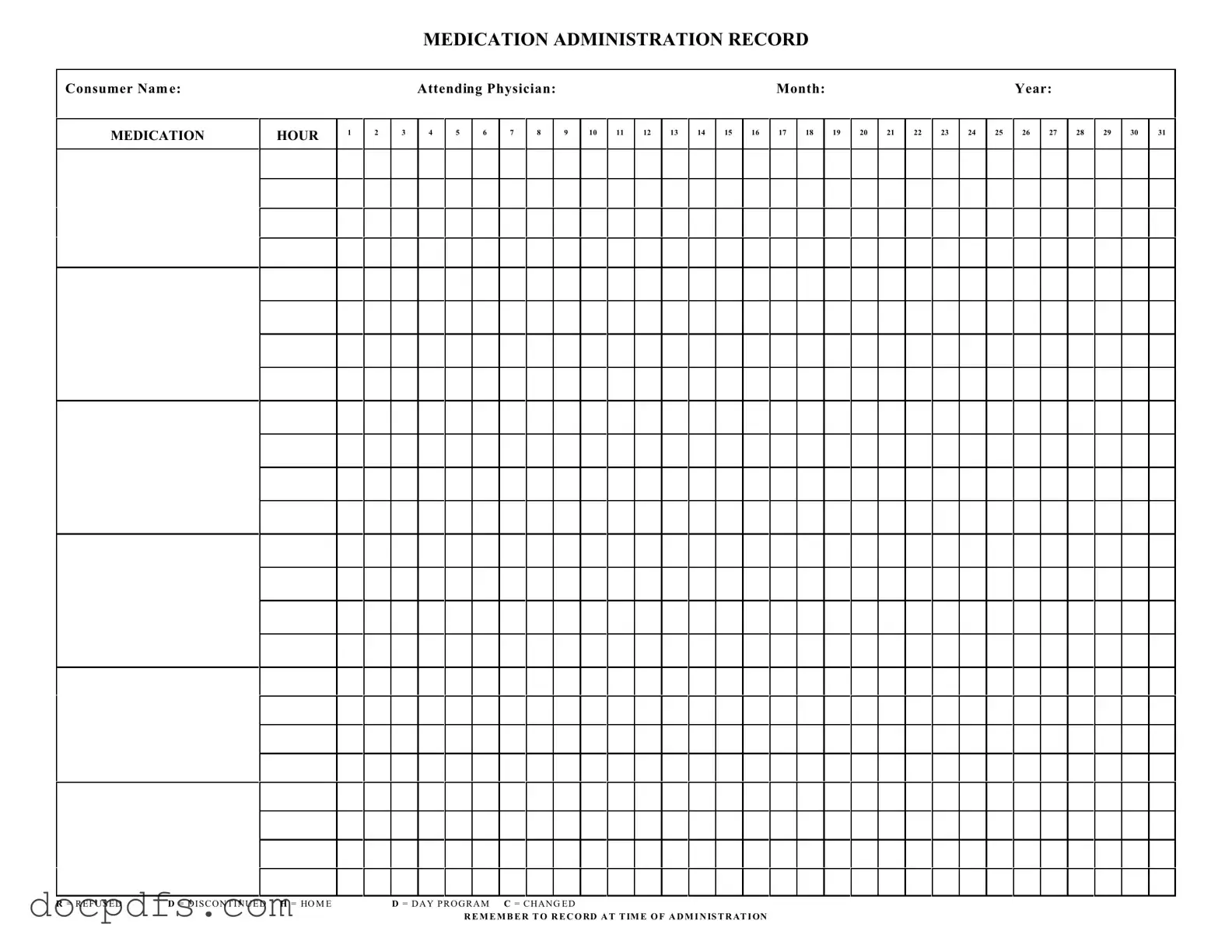
Medication Administration Record Sheet Template in PDF
The Medication Administration Record Sheet is a vital document used to track the administration of medications to consumers. This form ensures accurate record-keeping of medication doses, times, and any changes in treatment plans. By maintaining this record, healthcare providers can ensure that patients receive their medications as prescribed and monitor their overall health effectively.
Open Medication Administration Record Sheet Editor Now
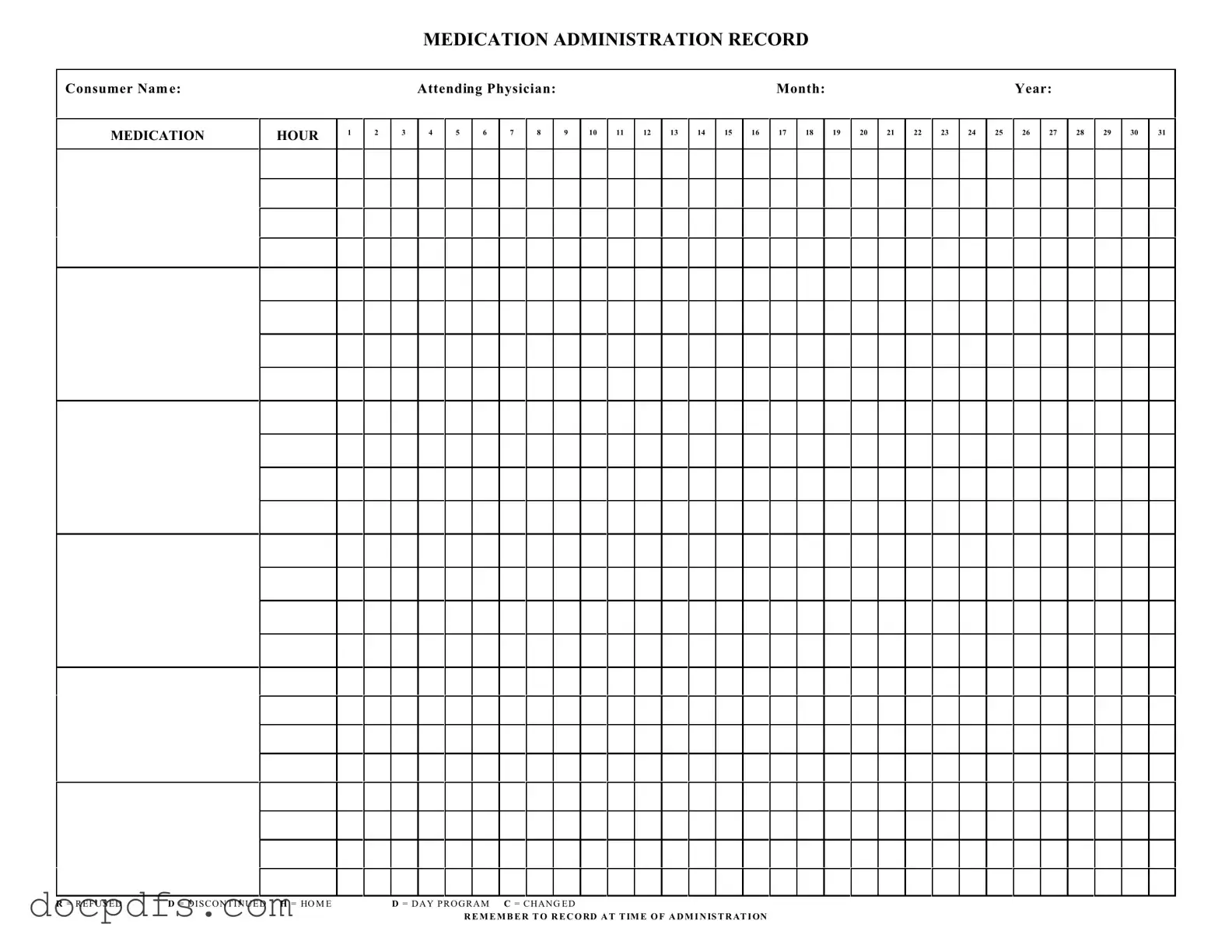
Medication Administration Record Sheet Template in PDF
Open Medication Administration Record Sheet Editor Now
Open Medication Administration Record Sheet Editor Now
or
⇓ Medication Administration Record Sheet
Finish this form the fast way
Complete Medication Administration Record Sheet online with a smooth editing experience.