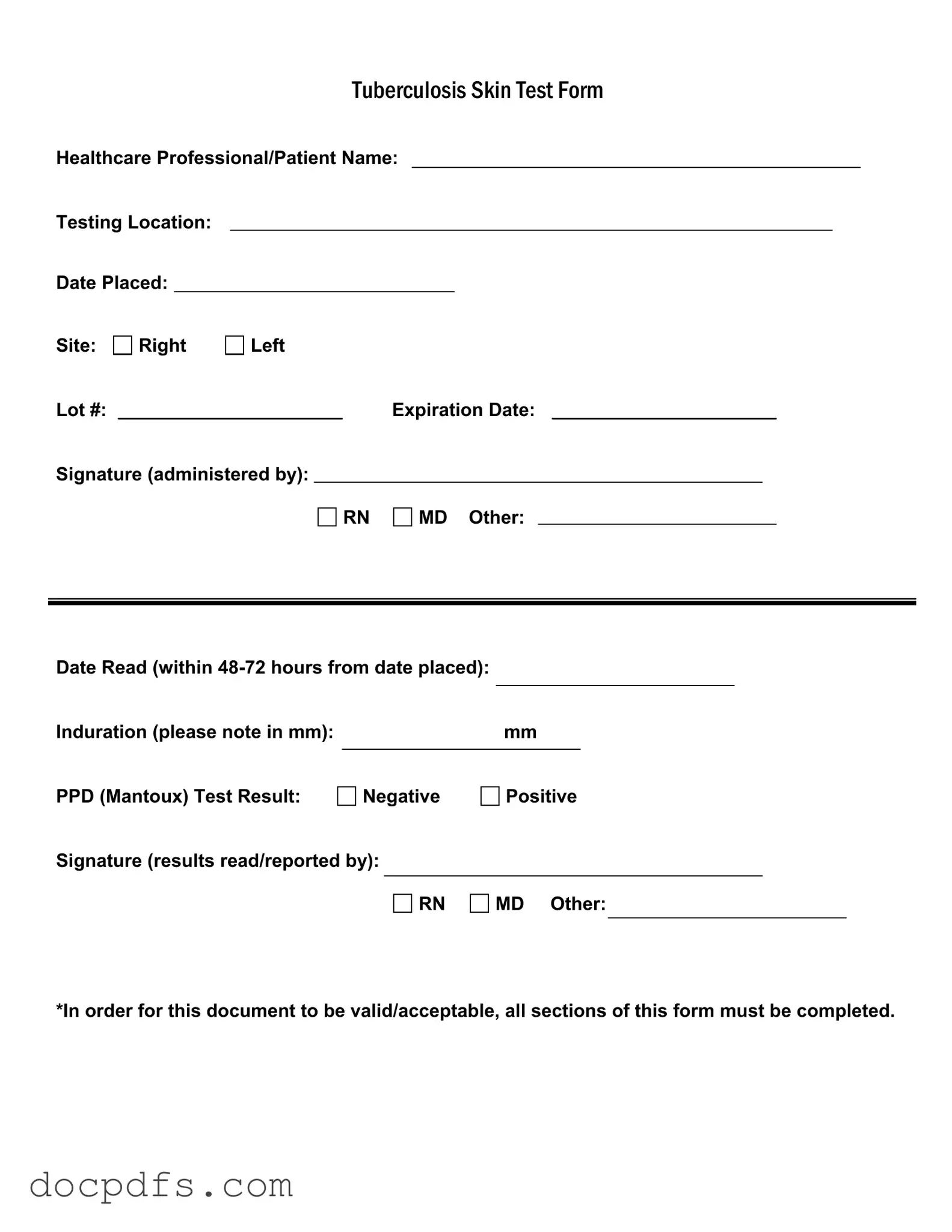
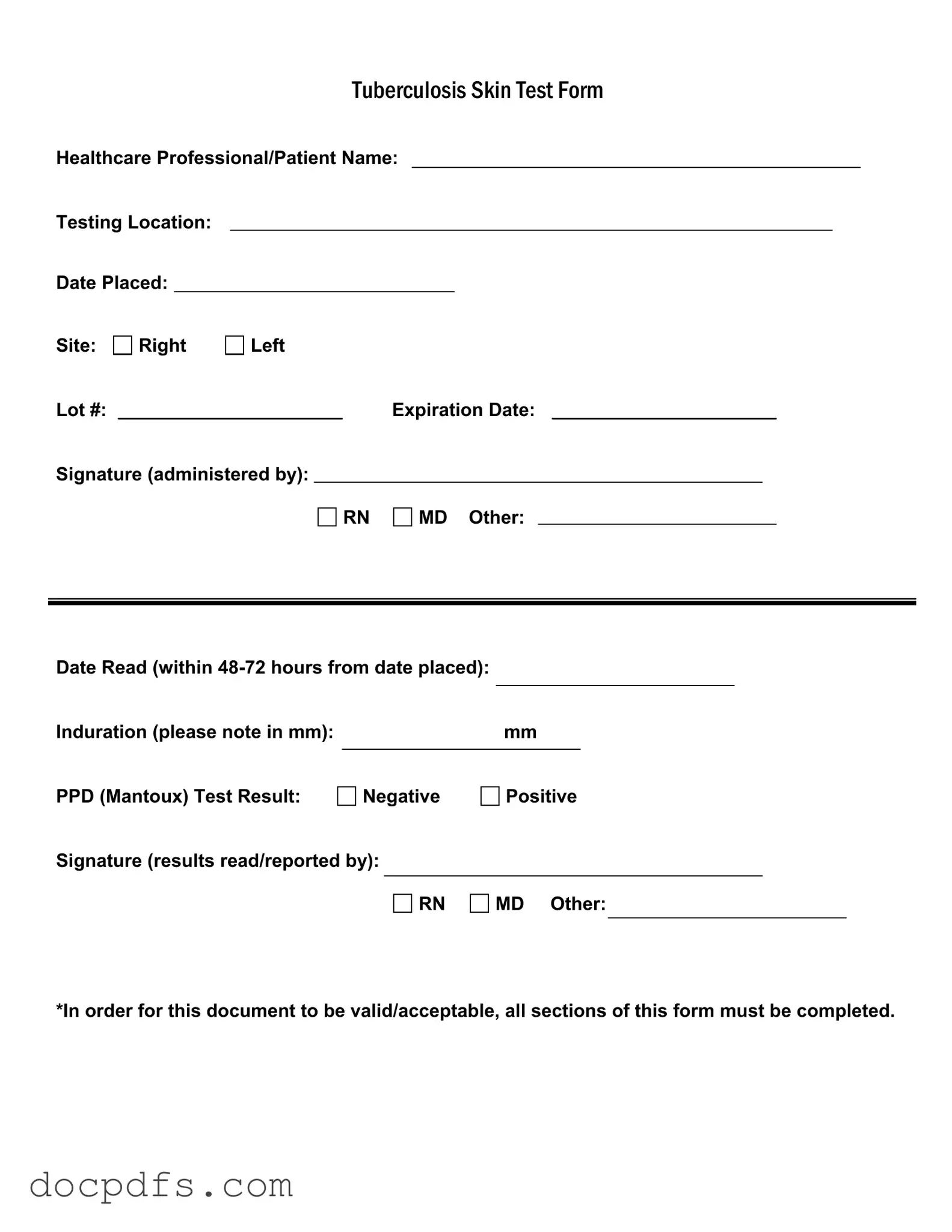
The TB Test form is used to document the administration and results of the Tuberculosis (TB) skin test, also known as the PPD (Purified Protein Derivative) test. This form ensures that all necessary information is recorded accurately, which is crucial for patient care and follow-up.
Who can administer the TB test?
The TB test can be administered by qualified healthcare professionals, including Registered Nurses (RNs), Medical Doctors (MDs), and other certified personnel. Their signatures on the form validate that the test was conducted properly.
To ensure the form is valid, all sections must be completed. Required information includes:
-
Healthcare Professional/Patient Name
-
Testing Location
-
Date Placed
-
Site of injection (Right or Left arm)
-
Lot number and expiration date of the PPD
-
Signature of the administering professional
-
Date Read (within 48-72 hours from date placed)
-
Induration measurement in mm
-
Test result (Negative or Positive)
-
Signature of the professional reading the results
When should the TB test results be read?
The results of the TB test must be read within 48 to 72 hours after the test is administered. This time frame is critical to accurately assess the induration, which indicates a reaction to the test.
What does the induration measurement indicate?
Induration refers to the raised, hardened area at the injection site. The size of this area, measured in millimeters (mm), helps determine the test result. A larger induration may indicate a positive reaction, suggesting possible TB exposure, while a smaller measurement may be considered negative.
What does a positive TB test result mean?
A positive TB test result indicates that the individual has been exposed to the bacteria that cause tuberculosis. However, it does not necessarily mean that the person has an active TB infection. Further evaluation, including a chest X-ray and medical history review, is often needed to confirm whether the person is infected.
What should I do if I have a negative TB test result?
If your TB test result is negative, it generally means that you have not been exposed to the TB bacteria. However, it's important to continue monitoring your health and follow any additional recommendations from your healthcare provider, especially if you have risk factors for TB.
The TB Test form itself does not have a specific expiration date; however, the results are typically considered valid for a certain period, often one year, depending on the requirements of schools, employers, or healthcare facilities. Always check with the relevant institution for their specific guidelines.
If you lose your TB Test form, contact the healthcare provider or facility where the test was administered. They may be able to provide a duplicate or a new test if necessary. Keeping a personal record of your health tests can help avoid such situations in the future.